Oh, newborns. So exciting and cute. So freaking complicated and scary. I mean, all of nursing is complicated and scary, but babies, especially. Because they're small. And fragile. And weird. Their circulation is weird, and their breathing is weird, their vital signs are weird. They're wet. And slippery. And floppy. And you have to poke and prod and test their Moro reflex, which makes them cry, and you just about lose your shit because evolution has wired us to want to give babies whatever they want to make them stop crying.
Before we get into APGARS (yay, more to memorize...)
Newborn VS:
HR: <100 if sleeping, 110-160, up to 180 when crying. Protip: I find tapping my finger while counting their tiny apical pulses for a full minute helpful with babies because otherwise I lose count.
Respirations: 40-60, usually shallow and irregular. There is transient apnea, but the apnea should never be more than 20 seconds. Look for nasal flaring, intercostal/supra/subcostal retractions, or see-saw breathing.
Temperature: 99.7-98.9F axillary. Temperature instability is a sign of infection.
BP: 60-80/40-50. Hypotension=sepsis/hypovolemia; Hypertension coarctation of aorta.
So, you delivered the head, cleared the mouth, then the nose (the mouth first to prevent aspiration), delivered the rest of the body, cut the cord, now what?
Apgar was named after the person who invented it (Virginia Apgar), yes, but more importantly, APGAR stands for:
A: Appearance completely blue (0); acrocyanosis (1); completely pink (2)
P: Pulse zero (0); <100 (1); >100 (2)
G:Grimace (with stimulation) no response (0); grimace (1); crying (2)
A: Activity (is the baby flexed) limp (0); some flexion (1); well flexed (2)
R: Respiration: zero (0), weak/<40 (1); good cry/>40 (2)
The numbers you need to remember with APGAR are: 4 and 8. 4 (repeat 4, 4, 4, 4, 4, 4) and up is moderately distressed (3 and down is severely distressed), 8 and up is WNL. APGARS are taken at 1 minute and 5 minutes after birth, and only again at 10 minutes if the child does not improve/is still below 7 at 5 minutes. Note, the stimulation for grimace is just drying the baby and getting him warm.
Once that is complete, the baby is printed and secured with an identity band for mom, dad (or mom mom or dad dad or whatever), and baby. And as long as baby is stable, we can begin feeding immediately after birth, and every 2-3 hours after with breastfeeding, and 3-4 hours with formula (formula digests slower, and you have to burp them ever 1/2 ounce or 1 ounce, and you have to chuck it after 1 hour of being prepared to prevent bacterial contamination). Here is proper latch on positioning, note the football position for C-section moms. We want a minimum of 100mL/kg in the first 24 hours. So, for example a 6 pound baby would be 2.7 kg x 100 mL/kg=270 mL.
[FYI: 16 ounces/1lb
so, if the baby is 6lbs 7 ounces
that's 6pounds + (7ounces/16ounces in a pound)= 6pounds+ 0.43pounds=6.43 pounds
--> convert to kilos
6.43pounds/2.2pounds per kilo=2.9kilos
--> multiply that times 100 mL/kg in the first 24 hours
=290 mL
but if they give you a problem, then the creator of that question is an asshole.
But you might have to calculate that in real life.]
GU: the baby needs to pee within the first 24 hours of life, and after the 4th day of life, urination occurs 6-10 times a day. They usually poop within 48 hours. Poop usually looks yellow and seedy. Teach that circumcised penises can be cleaned with warm water, and to apply petroleum jelly with each diaper change (q 4 hours minimum), and that yellow mucus is ok and to leave it on. It should heal in 2 weeks. Don't submerge the kid in a bath until then, cause the umbilical cord has to dry and fall off first (and you just clean that with a neutral pH cleanser and sterile water at birth, but otherwise it should remain dry until it falls off).
For the Ballard Score go here. I'm not going to memorize that because I don't have time for that.
Standard care and labs for newborns include:
- eye prophylaxis with erythromycin (for GCCT--aka gonorrhea and chlamydia) within the first hour of birth
- vit K IM injection within the first hour of birth
- Hep B within the first 12 hours.
- ABO Rh type and screen
- PKU
- CBC:
- RBC 4.8-7.1 million
- Hgb 14-24, Hct 44-64
- WBC 9-30,000
- platelets 150,000-300,000
- glucose 40-60 (within 2 hours of birth)**
- bilirubin day 1: 0-6; day 2: <8; day 3 <12; hyperbilirubinemia >15 at any time
Any time a baby is stressed (from withdrawal, from cold, from illness, from RDS) it will burn more calories. It is important to check glucose (hypoglycemia=2 consecutive <40 in term, <25 in preterm--remember preterm is before 36 6/7 weeks). Babies with hypoglycemia are jittery, cold and clammy, and eventually become flaccid and/or have seizures and slip into a coma--AND IT HAPPENS QUICKLY.
Transitional Periods
After the baby is born, it has 3 transitional periods: 1) first period of reactivity=first 30 minutes of life, which is the best time to breastfeed, 2) sleep from 30 minutes to 2 hours old, 3) second period of reactivity from 2 hours till 8 hours, where gagging and vomiting usually occurs, and then they feed again. (Awww, so cute.)
Guthrie test:
 |
| http://www.homebirth.net.au/wp-content/uploads/2010/02/new+born+screening-450x237.jpg |
Phenylketonuria
Every baby is tested for phenylketonuria 2 days after birth by federal mandate, with the Guthrie test (heel stick) which is a genetic condition where the baby cannot break down phenylalanine from protein into tyrosine. The infant starts off with failure to thrive, vomiting, irritability, hyperactive/erratic behavior and ends up with brain damage (older children display schizoid behavior like catatonia, screaming, biting, and head banging). Treatment means a protein restricted diet with no sweetners for life, and the baby must have a special phenylalanine-free formula (like Phenex-1).
Substance Dependent Babies
Fetal ETOH syndrome: Since ETOH is a depressant, the lack of a depressant will result in an irritable baby, crying, seizures. Other problems are IUGR, smaller/thinner/flatter than normal craniofacial features, and possible deafness.
Nicotine: premature, low birthweight, increased COPD (bronchitis, pneumonia), developmental delays, and increased risk of SIDS.
Opioid: sneezing, poor temperature regulation, hyperactive Moro reflex, CNS irritability-->seizures (especially with methadone).
Cocaine: shrill cry, tremors, sleeplessness, muscles spasms, feeding problems.
Often phenobarbital is prescribed for seizures. Decrease stimuli, swaddle, small frequent feedings of high calorie formula (possibly gavage). Many struggle with poor sucking of they can settle down enough to eat at all, so preterm nipples with larger holes are used, but try to breastfeed because it has been found to help ease withdrawal symptoms (the drugs carry over, especially if mom is on methadone to help kick the habit).
Premature Babies (<38 wks)
Premature babies have a low birth weight, little fat (brown fat deposits insufficient, which increases impact of cold stress or oxygen deprivation stress so cluster care and keep the baby warm), long periods of apnea (10-15 seconds), and may not be able to suck/gag/swallow/cough (before 34 weeks) so will require parenteral nutrition. Also, the child may suffer from RDS.
Respiratory Distress Syndrome
Occurs with premies, babies with meconium aspiration (aka perinatal asphyxia or stress asphyxia), and with C-section babies because they haven't had enough surfactant produced (premies), or they have fluid in their lungs (part of the compression of the torso required to pass through the pelvis squeezes out the fluid from the lungs and helps the baby draw its first breath). Oftentimes they will have intercostal or substernal retractions, nasal flaring, grunting, rales, cyanosis, etc. So, administer beractant (a synthetic surfactant), and don't suction for 1 hour so it can spread across the inside of the lungs.
Post-term Babies (>42weeks)
Post-term babies are at risk for injury during delivery (shoulder dysotcia, fx clavical, brachial plexus injury, or facial paralysis), possible risk of degenerating placenta causing meconium aspiration, hypoglycemia, and jaundice. Initiate early feeding, and watch for signs of pneumonia or jaundice.
Hyperbilirubinemia
(Bilirubin >15)
There are two types of jaundice: physiologic ("natural" or "expected") and pathological (has a disease process). Physiological jaundice occurs gradually (>24 hours later), and is caused by the natural breakdown of extra RBCs from mom. Also, it can happen because newborns have immature livers (less clotting factors), and there is a lack of Vit K. Pathological is jaundice that sets in within 24 hours of birth and/or lasts more than 7 days, and has an increase in bilirubin at 5mg or more a day, and is caused by blood incompatibility between the mother and the child, or from an infection, which can lead to kernicterus (brain damage due to bilirubin >25). Direct Coombs to test for sensitized RBCs. Treat with phototherapy (break q4hr to unmask eyes and check for inflammation or injury)--keep the kid naked, except for the genitals, and protect from burns (no oils or lotions), dehydration (lots of water), and hyperthermia. Feed the baby frequently to excrete bilirubin in stools (will look loose and green). If the baby is at risk for kernicterus (bilirubin >25), you may have to give an exchange transfusion. Kernicterus starts with the same stress symptoms as any other disease (lethargy, poor feeding, temperature instability, and hypotonia-->progresses to fever, seizures, and high pitched cry, and will result in cerebral palsy, mental retardation, upward gaze paresis, and hearing loss.
An easy way to remember risk factors for hyperbilirubinemia in full term infants is the acronym
Jaundice <24 hrs after birth (physiological)
A sibling who was jaundiced as a neonate
Unrecognized hemolysis (incompatibility--remember, Rhogam @28 weeks and at birth or any trauma), or delayed cord clamping=increased blood volume
Nonoptimal sucking (slow GI=re-unconjugation of bili in the intestine goes back into the bloodstream)
Deficiency in glucose-6-phosphate dehydrogenase
Infection
Cephalohematomas/bruising during delivery
East Asian or Mediterranean descent
 |
| http://cardiovascularsystemud.weebly.com/uploads/8/2/1/2/8212050/5709166.jpg?822 |
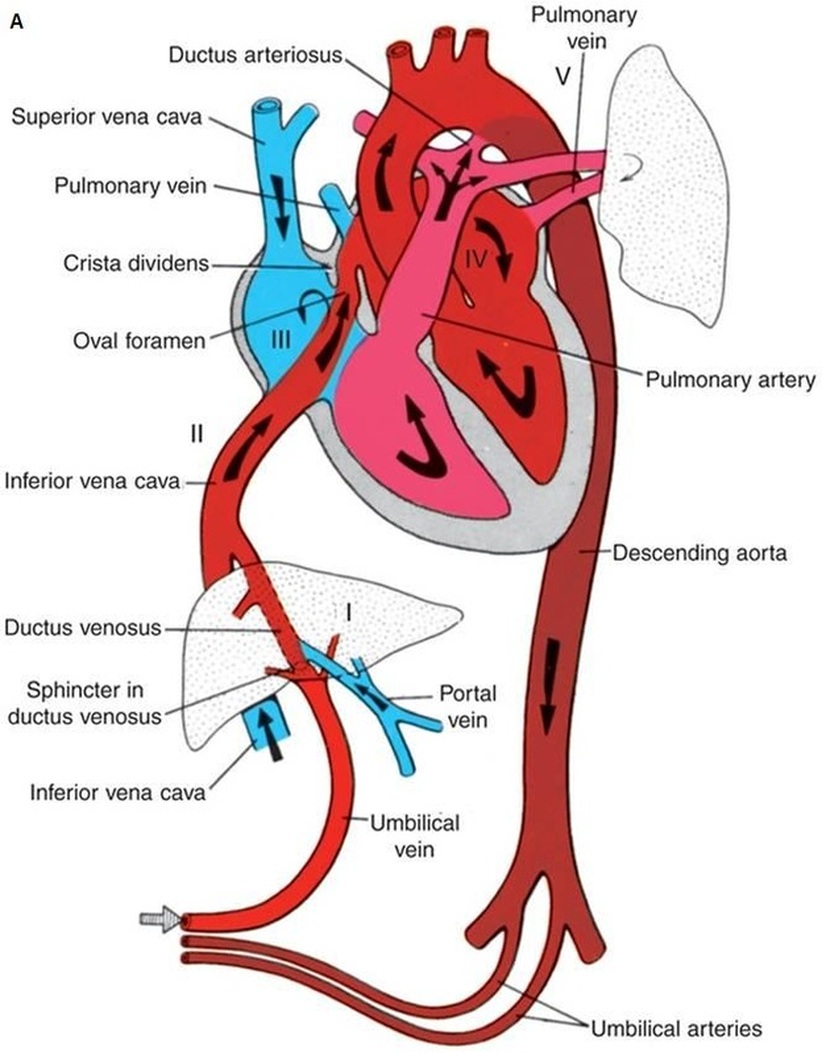
Almost all require surgical intervention except maybe PDA or ASD. These can be fixed with indomethacin which closes the holes. If left unfixed they all result in poor growth and development, and some degree of heart failure, and some of them (like TGV) result in death. Atrioventricular septal defects will result in a systolic murmur.
PDA 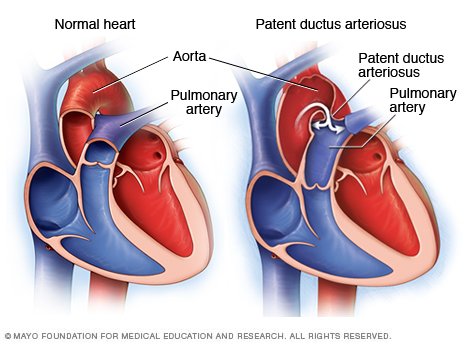 |
| http://www.drugs.com/mcd/images/image_popup/DS00631_IM01560_r7_patentductusthu_jpg.jpg |
PDA--the ductus arteriosus doesn't close. Most of the time it is asymptomatic, but sometimes there is a heart murmur and a wide pulse pressure because the aorta is getting a fuckload of blood from both ventricles, resulting in a high systolic. The left ventricle has to work super hard. Treatment: indomethacin and/or surgery.
Atrial Septal Defect (Patent Foramen Ovale)--The foramen ovale didn't close. The blood is bypassing the lungs. Treatment is surgery during preschool years (3-6 y-o).
Ventricular Septal Defect--Really large defects are called "Eisenmenger's complex." You'll hear a big systolic murmur, and heart failure. Small defects close spontaneously, large ones require surgery during preschool years.
 |
| http://www.drugs.com/mcd/images/image_popup/DS00615_DS00998_IM00438_r7_tetralogythu_jpg.jpg |
Tetrology of Fallot--1) Pulmonary stenosis, 2) VSD, 3) overriding aorta, 4) R. ventricle hypertrophy. This kid is seriously sick, and gets acute cyanosis and hypoxia called "tet" spells. Squatting helps to increase systemic vascular resistance, reversing the shunting and getting blood to the lungs and helping to oxygenated the blood. If this is hard to understand, put your finger over the aortic arch and imagine no blood can flow out that way (this is what happens with systemic vascular resistance). Now the blood has no where else to go when the ventricles pump *but* to the lungs. This kid usually has clubbing of the fingers and severe growth retardation. Surgery is necessary within the first few years of life.
TGV with ASD
 |
| http://static.bandbacktogether.com/media/images/2012/02/tgvdiagram.jpg |
Transposition of Great Vessels--This is the condition I personally call "I don't know how this baby survives 3 minutes after birth," because the aorta is connected to the right side of the heart, and the pulmonary artery is connected to the left side of the heart. The only way this baby survives is if it ALSO has VSD, ASD, or PDA, or SOMETHING that allows it to somehow circulate oxygenated blood between the two sides. It's insane. The treatment is to continue giving prostaglandins to keep the ductus arteriosus open and surgery is immediately done to swap the aorta and pulmonary artery back into the right place. It's absolutely insane.
Coarctation of aorta--So basically the aorta is narrowed, and the lower extremities don't get enough oxygen or nutrition. The left ventricle has to work extra hard to fight past that narrowing, causing heart failure. However, look at what those three little arteries at the top of the aortic arch flow to:
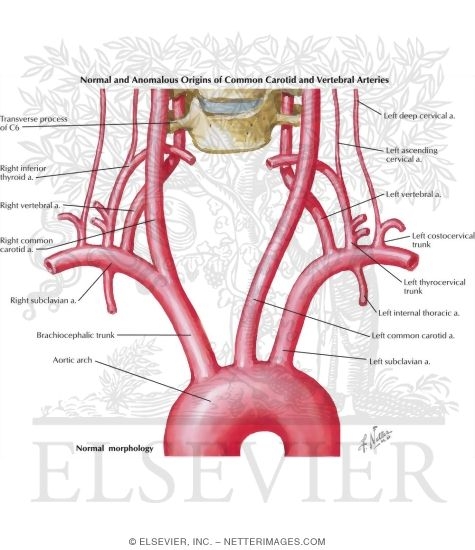 |
| https://www.netterimages.com/images/vpv/000/000/013/13922-0550x0475.jpg |
The nursing considerations for children with these congenital heart defects are: cluster care, provide small, frequent, high calorie meals with plenty of time to eat (gavage if necessary), avoid making the babies cry (I don't know how to not make a baby cry with gavage...). Observe for infection since these kids are at higher risk. Give medications to decrease the labor on the heart--like digoxin (0.5-0.8) hold if AP <90 (this is different than adults where the threshold is 60), Ca2+ channel blockers like captopril or enalapril, and duretics like furosemid or chlorothizide.
CONGENITAL ANOMALIES: SKELTAL
Clubfoot--To call clubfoot a purely congenital anomaly is a lie. The truth is we have no idea what causes it. Probably some sliding scale of genetics to intrauterine positioning. Club foot has 5 different manifestations you need to be concerned with:
 |
| http://odlarmed.com/wp-content/uploads/2009/04/talipes_clubfoot.jpg |
1) talipes equinovarus--the most common, with plantar flexion and feed bending midline. To help you remember the name, equin/o/varus means "the heel elevated like a horse" (hence "equine") and "turned inward" (hence "varus").
 |
| http://www.nursing-help.com/wp-content/uploads/2011/08/image60.png |
2) talipes calcaneus--the heel down and the toes up as if in permanent dorsiflexion.
3) talipes equinus--again, with the heel elevated like a horse.
 |
| http://www.nursing-help.com/wp-content/uploads/2011/08/image59.png |
4) talipes varus--as before, the toes turning midline
5) talipes valgus--the toes turning laterally
Whatever the cause, it is identified either with ultrasound or at birth. with radiography done to see the extent of the deformity. After the child is born, massage for lesser degree malformation can be used to manually straighten the foot/feet, or serial casting (changing the cast q2 weeks for 12 weeks) until maximum correction is achieved, and then application of a (rather medieval looking) Denis Browne splint or reverse last corrective shoes to maintain the correction. If the correction is too late, or not effective enough, surgery with ORIF may be required between 3-12 months of age.
Danis Browne splint:
| https://upload.wikimedia.org/wikipedia/commons/8/83/Botas.JPG |
Yeah. I know. Scary as fuck.
The treatment for hip dysplasia is a Pavlik harness that prevents hip extension or ADduction for infants <6 mos, and Bryant's traction and surgery to reduce with infants >6mos (or the Pavlik harness didn't work) with the addition of a hip spica cast.
So the basic care of both hip spicas and long leg casts (in the case of genu varum/valgus, or clubfoot), is ABC (checks q15) and by not applying the cast too tightly or smushing it while its drying, infection/skin care from pressure sores, etc. (you can apply "petals" of padding with tape around the edges of the plaster--especially around the window where urine and defecation take place), and also pain and psychosocial distractions for the baby, and nutritional needs (constipation from reduced movement). The parent may also need special strollers or car seats.
CONGENITAL ANOMALIES: NEUROLOGICAL
***Remember that AFP, or MSAFP is something you *screen* for in the first trimester with an integrated first trimester screen along with Tri21 and Tri18, and in the second trimester with quad and penta screens. Normal AFP is <2.5 MoM for singlets.
Neural tube defects--There are three main levels of neural tube defects you need to be concerned with: occulta, which is where everything is still sealed, meningocele, which is where the meninges is still intact and there's just a little bubble protruding out of the back, and myelomeningocele or "spina bifida," which is when there is an open spinal defect and the meninges (remember the meninges are the three layers of spinal membrane covering the nerves that encase the spine and the brain into one sac) are open and the spinal fluid and nerves are all spilling out.
Complications are hydrocephalus, clubfoot, scoliosis, congenital hip dysplasia, bowel and bladder problems...
Treatment is prevention (all women of child bearing years should take folic acid supplements since the spine fuses by week 10 and often times people don't know they are pregnant until after 10 weeks). After the child is born the treatment is surgery.
The nurse's job presurgery is to preserve the integrity of the meninges by keeping the infant prone and covering the protrusion with sterile saline moistened gauze. You don't cover the sac with clothes or diapers, and you have to be careful to clean the perineal area well to prevent tears or cracks in the meninges or the development of meningitis. Note that children with NTDs have an increased risk for latex allergy. Postsurgery, keep the infant in prone, monitor for IICP and hydrocephalus. If the child's injury causes bladder and bowel nerve damage, teach the parents CRede's maneuver and the child how to self-catheterize around age 5-6. Oftentimes the patient won't be able to feel if she has a UTI, so it's important to teach monitoring for infection (foul smell, cloudy urine, temperature).
Hydrocephalus-the imbalance of absorption of production of CSF inside of the cranial cavity, and/or the obstruction of the flow of CSF through the ventricular system. Sometimes, hydrocephalus develops later in life due to a malformation such as a neoplasm, infection, or trauma.
The infant will have increased head circumference with bulging anterior fontanels and distended scalp veins. They will be irritable, have a high pitched scream, and it is extremely uncomfortable for them to be cradled horizontally. Children with hydrocephalus like to be held upright--this relieves pressure from their cranium. An older child may verbalize headaches, blurry vision or diplopia, vomiting in the morning, and even experience seizures.
This kid needs seizures precautions both pre and post-op for realz, and constant neurological checks (like we said before, for children, it is measuring thee circumference of their occiptal frontal region). After the surgery you position the baby on the non-shunt/non-surgery side (you can use a wedge to keep them tilted up on one side), and watch their VS. like a hawk. Watch for sudden changes in consciousness, vomiting, and sudden increase in difficulty with feeding. Also, for infection--cause, you know, meningitis is bad. Also, teach the family TO WASH THEIR DAMN HANDS when handling the kid especially when pumping the shunt to relieve CSF pressure.
Cerebral Palsy-at it's most basic qualification, cerebral palsy is abnormal muscle tone and lack of coordination with spasticity (often with contractions) either of diplegia (both legs), hemiplegia (one side of the body), or quadriplegia (all 4 limbs). These children often have delayed milestone development and have a lot of back arching and dystonia or ataxia, but little other spontaneous movement including sucking and swallowing (so feeding can be challenging). Often these children have intellectual, visual, hearing, speech and language deficits, and can have seizures. Most cases of cerebral palsy are due to brain insult, whether in utero, during delivery, or after birth (such as sepsis or hyperbilirubinemia or PKU, infections like with meningitis/encephalitis like with spina bifida, toxins, or stroke). Obviously we stop whatever is the offending situation (give mom O2/side lie/stop the pit/emergency C/S, treat infection with antibiotics, give an exchange transfusion, etc.), but after birth, you just treat the symptoms (seizure medication, OT, PT, speech therapy and modify the environment)
Yeah. Scary as fuck. You still with me?
Okay.
CONGENITAL DISORDERS: GASTROINTESTINAL
The first two are easy to differentiate: Hypertrophic pyloric stenosis and Cleft lip/palate
Hypertrophic pyloric stenosis- is a thickening of the pyloric sphincter that may show up as an olive-sized mass in the upper right quadrant of the abdomen. Failure to thrive, projectile vomiting, and constant hunger are positive signs, plus an U/S to confirm. The child will have to undergo surgery and have an NG tube and be NPO until bs returns. Things to teach the parents include: side lie with head elevated when vomiting, watch for dehydration, assess the incision for infection, and otherwise hold the kid and give pain medication when the child seems to be indiscomfort.
Cleft-lip/palate--The test question material that always gets me with cleft-lip/palate is to maintain nutritional intake with a soft, elongated, or premie nipple, or with mom breast feeding because it fills in the cleft. A last resort would be NG tube or parenteral feeding. The baby should be fed in an upright position with frequent burping to prevent eustachian tube infection and extra gas. And the baby should be fed no less than four hours before surgery. After surgery, the suture integrity needs to be maintained with cleansing with normal saline or sterile water and sterile technique (seriously? it's the inside of the mouth...ok) and a cotton swab, or half strength peroxide if a crust has formed. Feed with an Asepto syringe or dropper to the side of the mouth, and suction gently and lay the baby on its back, but preferably on its side to maintain airway patency and avoid rubbing the stitches. Antibiotics and pain medication.
See? Stitches. Laying the baby on its face is a stupid idea.
 |
| http://67.199.56.100/adam/dochtml/graphics/images/en/7057.jpg |
Here's where the confusion occurs:
NTD is PRONE. Cleft-lip is SUPINE or SIDE.
Kind of duh, but I panic and mix them up on the test all the time.
Maybe I'm just stupid.
The next two are more similar: Hirschsprung's (which should just be called "congenital aganglionic megacolon," because "Hirschsprung" doesn't help a person remember a single thing about this disease) and Intussusception.
Hirschsprung's- Basically, part of the large intestines doesn't have nerves (aganglionic), so it doesn't have peristalsis. Think about a moving walkway in an airport. Say you throw a whole bunch of baggage on the moving walkway, but that section of regular floor between two moving walkways doesn't move, so the baggage piles up at the end of the moving walkway part, and then everything gets backed up. That's Hirschsprung's. Fluids will flow around the blockage, so you'll get diarrhea, but otherwise things back up so much the kid ends up projectile vomiting. There's a lot of pain, too, and peristalsis waves that are visible to the naked eye (cause the kid will be skinny from malnutrition), and worn down enamel from throwing up constantly. Treatment is: serial rectal irrigation to decompress the bowel, then surgery to resect the aganglionic section, then possibly a colostomy and NG-tube/NPO for a bit until the intestines recover. And antibiotics and pain medication.
Intussusception:
 |
| http://giphy.com/gifs/animated-illustration-motion-study-XhxVN2AQxB4LC |
Intussusception- Imagine the intestines fold on each other like a captain's spyglass being collapsed. It happens most often at the ileocecal valve and is accompanied by sudden and with acute pain with "currant jelly stools" of blood and mucus. You diagnose with a barium enema (which may actually straighten things out by pushing the ileum back out of the colon). And you treat with air injections or barium enemas. If that doesn't work then you cut that section out. Also you give PPI's (omeprazole/pantaprazole), and H2 receptor antagonists (ranitidine), and of course, antibiotics and pain medication, and care for the incision site.
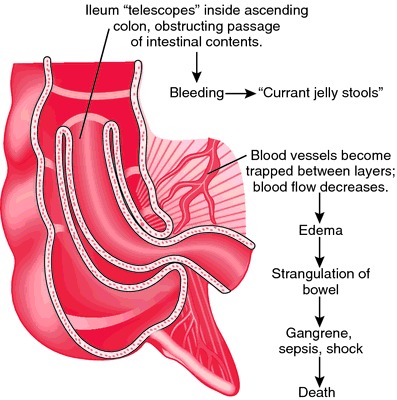 |
| http://img2.tfd.com/mk/I/X2604-I-26.png |
Don't know what currant jelly is?
 |
| http://www.dansukker.co.uk/files/Billeder/recipe_large/currant_jelly.jpg |
Yum.
Look, there's a million things we could cover, but things you really need to just know, VS, and that 1g=1mL of body fluid. A loss of 1kg=1000mL fluid loss, and that's a problem when you're a tiny person.

No comments:
Post a Comment